The Clinical Challenge
Performing surgery on fetuses whilst still in the womb poses many risks. Although pioneering work in this field began in the 1980s, it remains very challenging, with only a few highly trained teams around the world treating a handful of the most serious conditions.
Studies have proven that being able to perform surgery on the fetus whilst still in the womb offers better long-term outcomes for the child compared to post-natal surgery. However, performing open surgery (where the womb is opened) is an extreme option which has many side-effects, and current minimally invasive surgical tools and techniques are not suited to the unique environment inside the womb.
Some of the problems facing surgeons today include:
- Poor Visibility: the amniotic fluid is often cloudy and doesn’t offer the surgeon a clear-field of view
- Rigid Instruments: current tools for minimally invasive surgery are rigid. This means that unless the baby is in a certain position in the womb, which can’t be guaranteed, the surgery is very difficult to perform
- Multiple Incisions: current methods usually require three entry points for cameras and surgical instruments. Whilst fine for other surgeries, making multiple incisions to the womb can increase the risk of pre-term labour.
- Delicate Environment: as we cannot sedate the unborn baby during an operation, the surgeon must be able to operate to high precision on a moving object, which a much smaller degree of accuracy than in other surgeries.
- Limited data: current scans and pre-operative data do not provide the surgeon with accurate information such as the location of blood vessels in the placenta, or organ placement in the unborn child.
Our team are busy working on the challenges which we currently faced, with the specific medical conditions below in mind.
Medical conditions
-
Spina Bifida
For the purposes of GIFT-Surg, the surgery will focus on developing treatment for the most serious form of Spina Bifida Cystica – Myelomeningocele (MMS). MMS occurs when the protruding cyst contains tissue, spinal fluid, nerves and part of the spinal cord. The spinal cord is damaged or not properly developed. As a result there is always some paralysis and loss of sensation below the damaged region, but the degree of seriousness does vary.
Treatment of MMS attempts to repair the opening in the spinal cord and currently falls under three main methodologies:
1) Open Prenatal Surgery – Opening the womb to perform surgery on fetus pre-term: This surgery is not currently performed in the UK. It has high associated risks of maternal morbidity and pre-term labour. It is a high-trauma surgery to the mother as large incisions to the womb and uterus are made.
2) Postnatal Repair – Operating on the infant after birth: Operating after birth greatly reduces the risk of trauma to the mother and of causing pre-term labour compared to prenatal surgery. However, the impact of MMS is likely to be greater to the infant as many of the serious complications have already affected development irreparably whilst in the womb.
3) Fetoscopic Repair – Using specialised instruments to operate in utero: Performing the operation before birth reduces the impact of MMS by stopping many of the serious complicatio
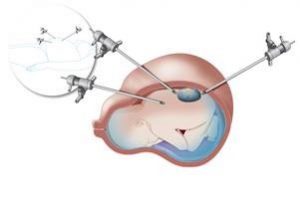 ns from developing and allowing a healing period within the protective environment of the womb, thus improving the long-term outcomes for the infant. The current operation requires 3 ports of entry, which poses a high-risk of pre-term labour and is technically difficult to achieve, and thus not recommended.
ns from developing and allowing a healing period within the protective environment of the womb, thus improving the long-term outcomes for the infant. The current operation requires 3 ports of entry, which poses a high-risk of pre-term labour and is technically difficult to achieve, and thus not recommended.How will GIFT-Surg help?
GIFT-Surg aims to develop the current methods used under fetoscopic repair by producing a miniaturised, multi-arm instrument which would need just one small (under 5mm), single-entry point into the uterus.
With improved precision and dexterity in comparison to current fetoscopic devices, it should allow for anatomical repair or application of tissue engineered repair using gels, combating the risks associated with current methods and offering improved outcomes. -
Twin-to-Twin Transfusion Syndrome
Twin-to-Twin Transfusion Syndrome (TTTS) is a disease that affects identical twins which share a placenta and some of the same circulation (monochorionic pregnancies). The shared placenta contains abnormal blood vessels and may also be shared unevenly. It can occur at any stage throughout the pregnancy, but the earlier in term has the greatest risks.
The condition results in the transfusion of blood from one twin (the donor) to the other (the recipient) in the womb. The donor twin is often underweight and anaemic, and the recipient twin can have a strain on the heart due to the increased blood supply. There can also be imbalances in amniotic fluids due to decreased bladder function in the donor twin, this can lead to ruptured membranes and early delivery.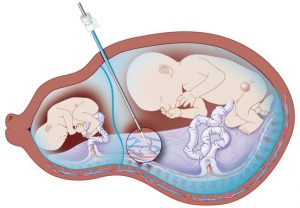
How is it currently treated?
Fetoscopic identification of the abnormal blood vessels (anastomosing vessels) on the placenta, followed by cauterization of these vessels with a laser.
Shortcomings of the current procedure include an inability for the endoscope and laser to operate at right angles when the placenta is located at the front of the womb, difficult visualisation and imaging due to cloudy amniotic fluid or small vessels on the placenta, uncertainty on classification of arteries and veins based on oxygen content and instability of imaging when carried out at close proximity due to movement in wombHow will GIFT-Surg help?
GIFT-Surg aims to develop technologies to improve the documented issues through:- Enhanced vision through photo-acoustic imaging
- Stabilisers and movement compensators
- An acute bending endoscope or lasering fibre
- Preoperative imaging and mapping to identify correct operative vessels
-
Congenital Diaphragmatic Hernia
Congenital Diaphragmatic Hernia (CDH) occurs when the diaphragm fails to form correctly during development (around 7-10 weeks gestation). This causes the the abdominal contents to herniate into the chest cavity, affecting lungs from developing properly.
The stage at which this occurs and the size of the hole in the diaphragm will determine the outcome of the condition and its affect on the organs of the unborn child.
CDH occurs in approximately 1 in 2500 births and accounts for around 8% of all major congenital abnormalities.
Fetoscopic Endoluminal Tracheal Occlusion (FETO) involves the placement of a balloon, via the fetal mouth and airway, into the trachea to enhance intrapulmonary pressure and encourage lung development. This is used in the treatment of upper airway obstruction conditions, such as CDH, which lead to life-threatening situations at birth.
At present, in utero airway management is limited by a lack of small flexible instruments with sufficient dexterity and pre- and intra-operative data fusion during treatment.
By developing the technology, tools and training for surgeons in order to improve the efficacy and ease of treatment of blockages by using the FETO method.
-
Lower urinary track obstruction
Lower urinary tract obstruction (LUTO), also known as obstructive uropathy, is a rare birth defect in which an obstruction of the urethra prevents or restricts the fetus from passing urine. Early diagnosis and fetal intervention can prevent life-threatening complications.
How is it treated?
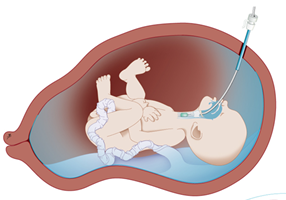
Fetal shunting: A shunt is a hollow tube that temporarily bypasses the lower urinary tract obstruction and provides an alternate passageway for urine to go from the bladder through the abdominal wall to the amniotic fluid space around the fetus. This allows for drainage of the urinary tract and bladder and establishes fluid around the fetus, which is necessary for lung development.
Fetal cystoscopy has been introduced to visualize the bladder neck area for diagnosis and treatment using lasers. Current limitations involve the acute angulation of the fetoscopic tip and laser fibre towards the bladder neck area.
How will GIFT-Surg help?
Research will focus on developing the advanced surgical tools necessary for early diagnosis and precise treatment for improved outcomes.